65 year old male a resident of ramanpet ,farmer by occupation came with chief complaint of SOB and neck pain since 1 week.
Hi, I am Y.Varunkarthik , 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
Chief Complaint
65 year old male a resident of ramanpet ,farmer by occupation came with chief complaint of SOB and neck pain since 1 week.
History of present illness
Patient was apparently asymptomatic 1 week back then he developed SOB which is grade -1 according to NYHA, relieved by taking rest. SOB increases after uptake of food, no orthopnea, no pnd and no pedal edema.
Neck pain since 1 week which was insidious in onset, intermittent type,no restriction of movements,non radiating pain , aggravated on exertion and relieved in medication.
No abdominal pain ,nausea and vomiting.
Past history
K/c/o hypertension since 10 years and on medication
K/c/o hypothyroidism since 10 years and on medication
N/k/c/o DM, epilepsy, asthma, cad, tb.
Surgical history :
Mesh herinoplasty 10 years ago.
Cataract surgery 10 years ago.
Treatment history :
Telmisartan 20 mg since 10 years. 40 mg for 2days
Personal history
Married
Mixed diet
Normal appetite
Regular bowel and bladder movements
Adequate sleep
Addictions - ciggerate smoking stopped 15 years ago(bedi).
Alcohol (toddy) -regularly
Family history -Not significant
General examination
Examination was done after taking consent from patient.
And examination was done in sufficient light occupied room
Patient was conscious coherent and cooperative
Moderately built
Moderately nourshied
Well oriented to place and time
Pallor present
No cyanosis
No clubbing
No lymphadenopathy
Pedal edema present - pitting type , extending upto knee .
Vitals
Temperature-afebrile
BP-150/90 mmHg
RR-19cps
PR-86/min
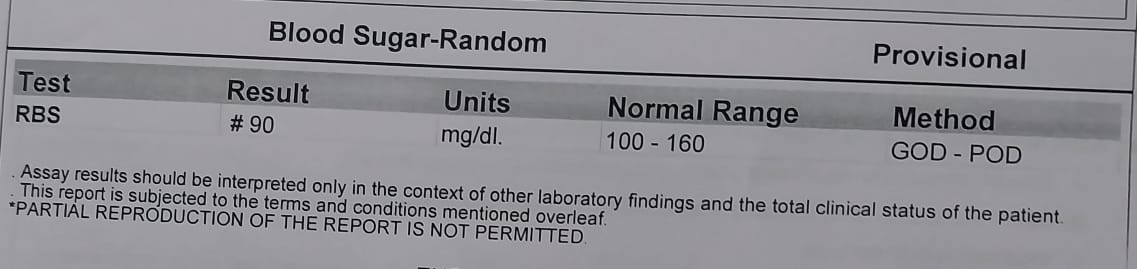
GRBS-99mg%
SPO2-99%
Systemic examination
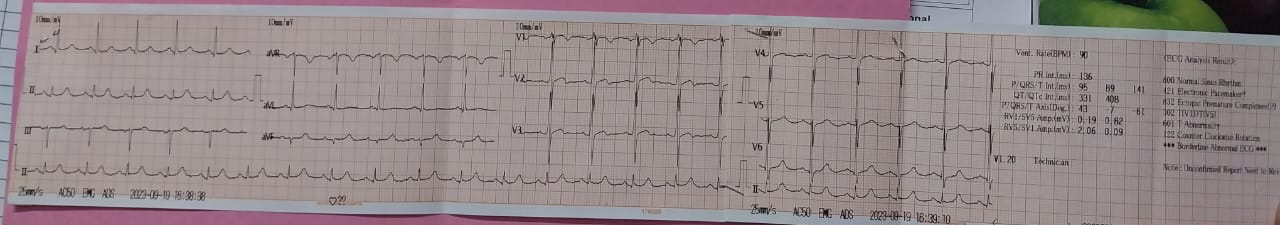
CVS:
No thrills
S1,S2 are heard
No murmurs
Respiratory examination:
- No Dyspnoea
- No wheezing
- central trachea
- Normal vesicular breath sounds
- BAE+
ABDOMEN
- abdomen - obese
- No tenderness
- No palpable mass
- non palpable liver and spleen
CNS
- conscious and coherent
- normal speech
Treatment
Tab.ultracet po/bd
Tab.telma 40 mg/ po/od
Tab PAN40 mg /od